How to improve your breathing
The link between dental health and breathing

Your dentist and respiratory problems
I am always looking for alternative methods that can improve the overall health of my patients, my team and my own. Natural options that involve lifestyle changes rather than taking medication or surgery are of particular interest to me. The Buteyko method is a set of exercises that can significantly improve the quality of breathing, thus health and general well-being.
The quality of our breathing has a huge impact on all systems in our body, especially the health of our mouth. Why? Because a healthy respiratory system keeps us away from cavities, tooth wear and general degradation of our beautiful teeth.
When a dentist detects a breathing problem in a patient, he must refer that patient to a specialist:
- Stuffy nose: otolaryngologist
- Suggested Treatments: corticosteroid nasal spray or nose surgery
- Other respiratory problems (eg obstructive apnea): pulmonologist
- Treatments proposed: C-PAP device and / or throat surgery
The breathing exercises of the Buteyko method
These approaches are effective in many situations, but are reserved for severe respiratory problems. What can be done for light or moderate problems?
Here is where the Buteyko method comes in. These breathing exercises offer the opportunity to improve the functioning of our respiratory system without medication, dental appliance or surgery. It suggests that breathing is the most natural and powerful medicine.
It can reduce symptoms of the following disorders:
- Anxiety
- Asthma
- Hypertension
- Chronic fatigue
- Allergies
- Attention deficit
- Snoring
- Sleep Apnea
- Insomnia
- Constipation
Dr Constatin Buteyko
Dr. Buteyko is a highly skilled Russian scientist who made his career during the Cold War. During his research, he discovered a link between the tidal volume of his patients and several diseases, including asthma. He was also a consultant for the Russian aerospace program during the 1950s: his goal in the program was to teach astronauts how to modify their breathing in order to consume less oxygen, and thus control the volume of oxygen tanks in rockets.
When he was studying his asthma patients, he discovered a feedback loop between breathing difficulties and excessive breathing. Not only do breathing difficulties cause excessive breathing, but excessive breathing can also cause breathing difficulties!
Excessive breathing, which is also called hyperventilation, creates breathing difficulties. This can be great news for those who are ready to improve their overall health: learning to breathe less can potentially improve your quality of life.
What are the symptoms of hyperventilation?
- Respiratory system: wheezing, shortness of breath, coughing, chest tightness, frequent yawning, snoring and sleep apnea.
- Nervous system: dizziness, lack of concentration, numbness, sweating, dizziness, tingling in the hands and feet, malaise, tremors and headache.
- Heart: rapid heartbeat, chest pain, and jerky or irregular heartbeat.
- Spirit: a certain level of anxiety, tension, depression, apprehension and stress.
Other general symptoms include dry mouth, nightmares, dry, itchy skin, sweaty hands, cramps, spasms, frequent urination (such as bedwetting or regular bathroom visits at night), diarrhea, constipation, general weakness and chronic fatigue.
The science of breathing
It is generally thought that the ideal breath relies solely on oxygen. According to studies derived from the Buteyko method, this could be wrong. 75% of oxygen is released at rest. Both gases are needed to optimize the oxygen supply:
Carbon dioxide: Not only waste, it has an essential role. It is used for the oxygenation of organs and muscles which allows oxygen delivery. It relaxes the muscles of the respiratory tract and arteries. Lack of carbon dioxide can cause contraction of blood vessels.
Nitric oxide: A major bronchodilator and vasodilator. An antibacterial agent that helps neutralize germs and bacteria. It makes the surface of the blood vessels less sticky to prevent cholesterol build-up.
To oxygenate our body, we must breathe less, not more.
Simplified Buteyko technique
Several experts offer programs to apply the Buteyko method. Here are the guidelines to help you determine if this method is right for you:
1. Practice athlete breathing.
You almost always breathe through your nose. You should never hear your breathing at rest. Stop sighing and stop taking deep breaths. Imagine how an athlete by your side would breathe – calmly and gently.
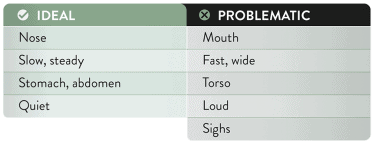
Want to know if your breathing is ideal or can improve? Here is a chart that can help you:
But what can people with stuffy noses do? Dr. McKeown, an international leader in the Buteyko method, suggests rinsing it with saline water and doing an exercise to clear the nose similar to the one in the following video:
2. Sleep with adhesive tape on the mouth.
How to avoid mouth breathing at night? Simply apply adhesive tape on your mouth. Here are some tips to make this new habit easier:
- Choose a medical tape, such as the “Micropore” from 3M.
- To avoid panic and a suffocating feeling at first, simply apply the tape when watching TV. If you are uncomfortable and you feel panic rise in you, simply remove the tape and try again the next day.
- When applying, fold up the edges and remove some of the adhesive to make it easier to remove the tape the next morning.
3. Exercise to increase your respiratory power.
Dr. McKeown offers exercises such as this one to improve your breathing (see video):
Following this introduction to the Buteyko method, which requires discipline and may discourage many, I invite you to read more on the subject and to consult the following research:
Bowler et el (1998) Buteyko Breathing Techniques in Asthma: A Blinded Randomised Control Trial. Medical Journal of Australia Vol. 169, pp.575-578. At 3 months the Buteyko group significantly reduced bronchodilator use by an average of 90% compared to 5% by control group. No significant difference between groups in hospital admission or oral steroid use. No change in oral steroid use or lung function in either group. Trial was criticised for providing greater input to Buteyko group compared with the control group.
Opat et al (2000) A Clinical Trial of the Buteyko Breathing Technique as Taught by Video. Journal of Asthma Vol. 37, No. 7, pp.557-564. Two groups of asthmatics, both groups watched a video twice a day for 2 weeks. The intervention group watched a Buteyko instructional video, the control watched a nature video. At 6 weeks the Buteyko group showed a significant decrease in bronchodilator use by 60% and significant improvement in quality of life, with improvements in breathlessness and mood. The control group increased bronchodilator use by 2.5%. There was no change in inhaled steroid use or lung function in either group and no difference in exacerbations, oral steroid use or hospital admission between groups.
Cooper et el (2003) Effect of Two Breathing Exercises (Buteyko and Pranayama) in asthma: A Randomised Controlled Trial. Thorax Vol. 58, No. 8, pp. 649-659. Compared Buteyko with the Pink City Lung Exerciser (a device which slowed expiratory flow) and a placebo group. The Buteyko group showed significant reduction in bronchodilator use and symptoms at 6 months, with no significant change in these variables in the other 2 group. There was no change in inhaled steroid use or lung function in either group and no difference in exacerbations, oral steroid use or hospital admission between groups.
McHugh et al (2003) Buteyko Breathing Technique for Asthma: An Effective Intervention. New Zealand Medical Journal Vol. 116, No. 1187. Designed to counter the criticisms of the Bowler et al, 1998 study. Bronchodilator use was significantly reduced in both both the Buteyko and the control group at 6 weeks, months and 6 months. However bronchodilator use was significantly lower in the Buteyko group than the control group at 6 weeks and 3 months. At all follow up points inhaled steroid use was significantly reduced in the Buteyko group, with no change in the control group. There was no change in quality of life or lung function in either group and no difference in exacerbations, oral steroid use or hospital admission between groups.
Slader et al (2006) Double Blind Randomised Controlled Trial of Two Different Breathing Techniques in the Management of Asthma. Thorax Vol. 61, pp. 651-656. Compared Buteyko with upper limb exercise combined with ‘controlled breathing’, which focused on relaxation and posture but not nasal nor hypoventilation. This was the first trial to advise the control group to use their exercises on the onset of asthma symptoms, prior to considering reliever inhaler use. Both groups significantly reduced their reliever use (86%) and steroid use (50%) at 3 months. Reliever free days increased from 6.7% to 53.5% in the Buteyko group and 8.3% to 55.3% in the control group at 3 months.
Cowie et al (2008) A Randomised Control Trial of the Buteyko Technique as an Adjunct to Conventional Management of Asthma. Respiratory Medicine Vol. 102, No. 5, pp. 726-732. The largest Buteyko trail to date with 129 participants. Buteyko vs. breathing control and relaxation. At 6 months the Buteyko group had significantly reduced their inhaled steroid use, with no change in steroid use in the control group. Asthma control (based on the Canadian asthma consensus report) had significantly improved in both groups with the Buteyko group control increasing from 40% to 79% and the control group increasing from 44% to 72%.
Prem et al (2013) Comparison of the Effects of Buteyko and Pranayama Breathing Techniques on Quality of Life in Patients with Asthma- A Randomised Controlled Trial. Clinical Rehabilitation. Vol. 27, No.2, pp.133-141.
The authors criticised Cooper et al, 2003 using the Pink City Lung Exerciser to mimic Pranayama (yogic breathing) as no preparatory breathing exercises or nostril breathing were included. A large trial of 120 participants. Three groups; control, Buteyko and Pranayama. At 3 months both the Buteyko and Pranayama groups demonstrated a clinically and statistically significant improvement using the Asthma Quality of Life questionnaire (within sub domains and total score). There was no significant difference between these 2 groups. There was no significant change in the control group. The Buteyko group was the only group to demonstrate a significant improvement in asthma control using the Asthma Control Questionnaire. There was no significant difference in moderate or severe asthma exacerbations between all groups.